It has already been established that COVID-19 is much more than merely a respiratory illness, and new research sheds light on how much it impacts another critical part of the body – the brain.
Almost one-third of the patients hospitalized with COVID-19 developed encephalopathy – a degeneration of brain function – according to a study by Northwestern Medicine in Chicago.
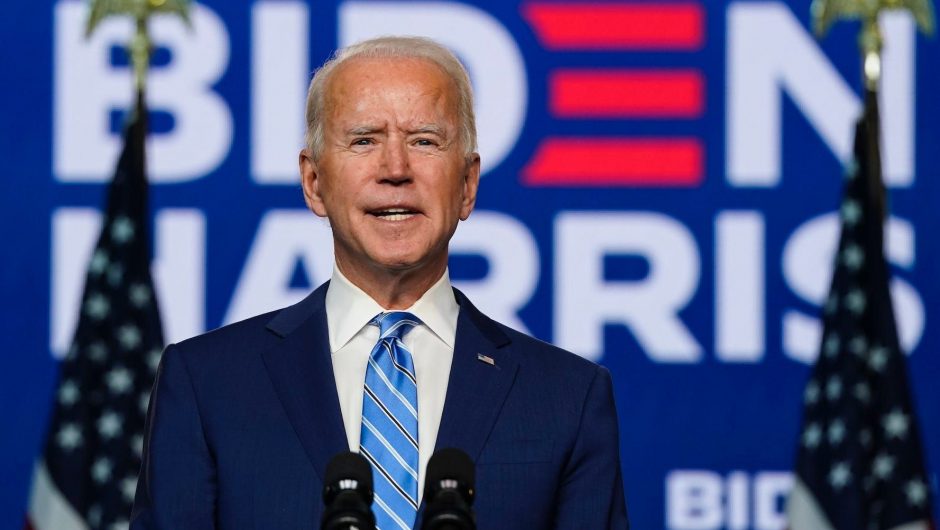
The finding raises serious national concerns in light of President Donald Trump’s recent three-night stay at Walter Reed National Military Medical Center, and on a larger scale, they also highlight the mental damage the coronavirus has inflicted on tens of thousands of Americans.
According to The COVID Tracking Project, more than 415,000 people in the U.S. have been hospitalized with the disease, which has killed more than 210,000 Americans among nearly 7.5 million infected by the virus.
WebMD describes encephalopathy – not to be confused with encephalitis, or swelling of the brain – as a group of disorders that represent “a serious health problem that, without treatment, can cause temporary or permanent brain damage.’’
“Encephalopathy, which is characterized by altered mental function ranging from mild confusion to coma, is the most severe neurologic manifestation of COVID-19,” said Dr. Igor Koralnik, a professor of neurology at Northwestern University who treats patients in the Northwestern Medicine health care system.
Koralnik is one of the authors of the study, the first one of its kind in the U.S., conducted on 509 COVID-19 patients within the hospital network in Chicago and its suburbs.
The research, published Monday in the Annals of Clinical and Translational Neurology, explored the neurologic manifestations of COVID-19 and found some were present in 82.3% of the patients at some point in the course of the disease.
Those symptoms included muscle pain (44.8% of all those reviewed), headaches (37.7%), encephalopathy (31.8%), dizziness (29.7%) and disorders of taste (15.9%) and smell (11.4%).
Story continues
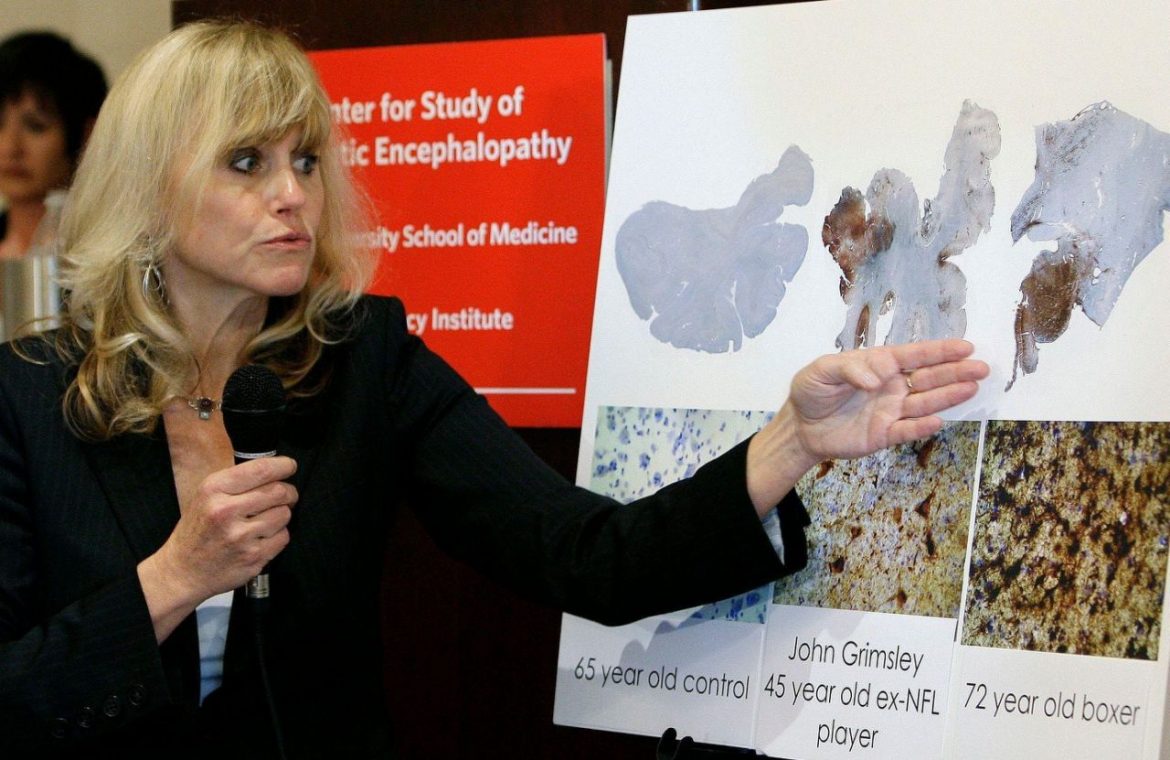
Dr. Ann McKee, of Boston University School of Medicine, has found chronic traumatic encephalopathy (CTE) in the brains of 90 former pro football players. (Photo: AP)
The scientists discovered that not only were patients with encephalopathy less able to take care of themselves – 32.1% of them had that ability after being discharged from the hospital, compared to 89.3% of those who did not develop that symptom – but they were also much more likely to die within 30 days of being admitted to the hospital (21.7% compared to 3.2%).
“Neurologic manifestations occur in most hospitalized COVID‐19 patients,’’ the analysis says. “Encephalopathy was associated with increased morbidity and mortality, independent of respiratory disease severity.’’
Dr. Richard Temes, director of the Center for Neurocritical Care at Northwell Health in Manhasset, New York, said that even though the study examined patients at hospitals in the Chicago area, the results are applicable nationally because COVID-19 “doesn’t respect boundaries, borders or geography.’’
Temes pointed out that most people who contract the disease won’t endure the harsh symptoms the researchers noted, but those who become critically ill – requiring a stay in an ICU and possibly sedation and use of a ventilator – are at the highest risk for those manifestations.
“This study highlights that for survivors of COVID-19, when they survive the infection, their recovery is just beginning,’’ he said. “These patients can have longstanding and lingering effects.’’
This article originally appeared on USA TODAY: COVID-19: Hospitalized patients prone to brain malfunction, study finds